What is the Proprioception Sensation?
The proprioception sensation is an important bodily neuromuscular sensation and falls under the sixth sense, more commonly known as somatosensory sensation. The term somatosensory or somato-sensory senses is a term that includes the subcategories of mechanical sensing, thermal sensing, nociception, sense of balance, proprioception and includes all senses. Feedback from all these different sensory components for higher processing originates from the peripheral nervous system and sends information to the central nervous system at both the spinal cord level and the cerebral cortex.
Proprioception Sub-Modalities
Proprioception itself includes several sub-modalities and these are as follows:
Proprioception (joint position sense): Proprioception is the sense of joint and limb positioning. Usually measured by joint position sensing, active joint position sensing (AJPS) and passive joint position sensing (PJPS). Joint position perception determines a person’s ability to sense the presented joint angle and then actively or passively reproduce the same joint angle after the limb is moved. It is also clinically measured as a joint matching task.
Kinesthesia: Kinesthesia is the awareness of the movement of the human body, that is, the sense of movement. The sense of motion refers to the ability to appreciate joint motion, including the duration, direction, amplitude, speed, acceleration, and timing of movements.
Sense of strength: Sense of strength (SoF) is also known as a sense of effort, weight, tension, or force-matching. It is the ability to reproduce or match a desired force one or more times. The sense of strength is thought to result from the afferent feedback of the Golgi Tendon Organs embedded in the tendons, muscle spindles in the muscles and proprioception in the skin.
Sense of change in velocity (SoV): SoV is the ability to perceive vibration derived from oscillating objects placed on the skin. It is believed to travel along the same type of large afferent nerve fibers as proprioception. It generally arises from the sum of neural inputs from joint capsules, ligaments, muscles, tendons and skin in a versatile system that affects all sub-modalities, the body’s behavioral regulation and motor control. Proprioception is critical for meaningful interactions with the environment, however, it helps to plan movements, sports performance, playing a musical instrument, and ultimately prevent an injury.
Its neurological basis comes primarily from sensory receptors located in the skin, joints and muscles. These muscle afferent receptors allow the definition of limb position and movement through the neural signal of a change in muscle, skin, or joint tension. Thus, proprioception is essentially a continuous loop of feed forward and feedback inputs between sensory receptors in the body and nervous system. A mechanoreceptor is a sensory receptor that responds to mechanical changes in tissues. There are different types of mechanoreceptors and they are as follows:
• Pacinian corpuscular
• Meissner corpuscular
• Merkel Discs
• Ruffini corpuscular
• Golgi Tendon Organs (GTO)
• Free nerve endings
However, there are also mechanoreceptors in the hair and skin. There are four types of mechanoreceptors found in ligamentous tissues. All mechanoreceptor types are myelinated and rapidly transmit sensory information to the CNS. The types of mechanoreceptors found in ligamentous tissues are as follows:
- Type I: Low threshold, slow adaptation (small) at both static and dynamic settings
- Type II: Low threshold, rapid adaptation to dynamic settings (medium)
- Type III: High threshold, slowly adapting to dynamic settings (large)
- Type IV: High-threshold pain receptors (very small) that warn of injury
However, it is believed that mechanoreceptors, particularly found in Type II and Type III ligamentous tissues, are associated with the individual’s sense of proprioception.
Causes of Proprioception Disorder
Poor proprioception in a joint can increase the likelihood of injury. The cause of proprioception disorders is currently unclear. It may result from decreased proprioception sense, local tissue damage, the presence of edema, or competitive nociceptive inputs. Proprioception can be affected by a number of factors, including:
• Temporary deterioration caused by a dangerous situation, eg alcohol consumption.
• Age-related changes also affect proprioception. The risk of loss of proprioception increases with age due to a combination of natural age-related changes in nerves, joints and muscles.
• Injuries or medical conditions affecting the neuromuscular system that can cause long-term or permanent impairment of proprioception.
Proprioception disorders have been noted among some neurological conditions. These neurological conditions are as follows:
• Brain injuries: Multiple sclerosis, stroke, Parkinson’s disease, Huntington’s disease, ALS
• Health conditions: Herniated disc, arthritis, autism spectrum disorder, diabetes, peripheral neuropathy
• Post-surgery: Operations for dental or hip replacement joint prostheses
• MSK conditions: Ankle sprains, ACL injuries, shoulder dislocations and tendinopathies, whip-related disorders.
Assessing Proprioception
Proprioception measurement is not fully developed today. And it can be safely measured in a laboratory environment using only sophisticated computer-interfaced equipment. There is a lack of valid, reliable, sensitive tools and outcome measures to measure proprioception deficiencies in a clinical setting. When a proprioception deficiency is suspected, focus should be on clinical aspects and these include:
The subjective assessment should include the following questions:
• Balance problems such as standing on one leg while walking or sitting or falling frequently
• Uncoordinated movements, such as inability to walk in a straight line or difficulty reaching an object
• Avoiding certain activities, such as climbing stairs or walking on uneven surfaces, for fear of falling.
Objective evaluation should include the questions in the subjective evaluation and observation of the following points:
• General coordination, reach tests, star wandering balance test, upper extremity coordination tests
• Incompetence, such as falling or hitting something
• Poor postural control, such as hunched over or putting extra weight on the table for balance while sitting
• Difficulty recognizing proper muscle strength for a task eg; Pressing too hard when writing with a pencil or inability to measure the force required to pick up an object.
There are several clinical tests that physiotherapists can use to evaluate proprioception depending on the body part being evaluated. These clinical tests are as follows:
Romberg test: Standing with shoes removed and arms crossed at the side or front of the body. The patient is asked to stand quietly, first with eyes open and then with eyes closed. And in this way, the patient tries to keep his balance. In addition, the Romberg test is scored by counting the seconds in which the patient can stand with his eyes closed.
Heel test: The patient is asked to touch the heel of one foot to the other knee, and then pull the heel down and back up in a straight line in front of the lower legs. This test should always be done in the supine position to counteract the effect of gravity on the heel moving down the shin.
Ataxia test: It is the test of keeping the finger of the examiner at the farthest point that the patient can reach and moving the finger of the examiner from time to time to a different place.
Alternating nose-finger test: The patient is asked to alternately touch the nose and finger of the examiner as quickly as possible.
Distal proprioception test: The person moves the joints of the hip, knee ankle and big toe up and down while watching the tester. He is then asked to repeat the same movement with the eyes closed.
Opposing joint matching task: The patient is asked to match a shown joint angle and measures the difference between the actual joint angle and the reproduced joint angle.
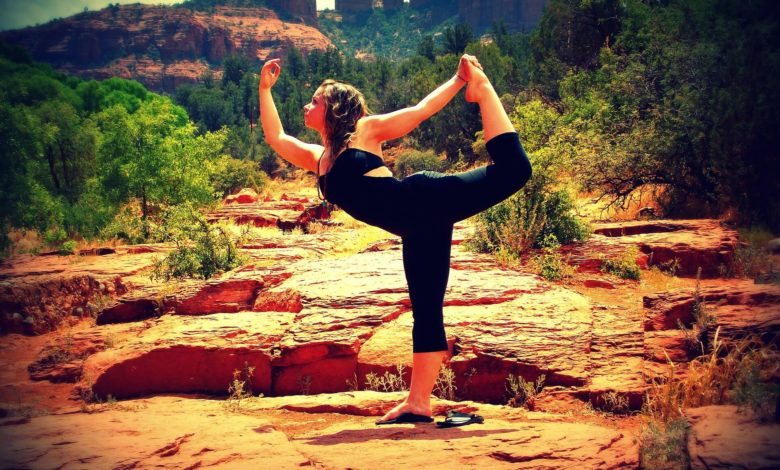
Learning New Skills
An intact sense of proprioception is essential to learning a new skill. During the learning of any new skill, for example sports performance or an artistic activity, it is often necessary to be familiar with some proprioceptive tasks specific to that activity. Without reasonable integration of proprioceptive input, an artist would be impossible to drive a vehicle unless he could paint without looking at his hand while moving the brush across the canvas. Because otherwise, a driver would not be able to control the pedal and steering while looking at the road ahead. As a result, proprioception is important for the training and development of emotion.
Physiotherapy-Proprioception Training
Regardless of the underlying cause of a proprioceptive deficiency, clinicians can rehabilitate patients with tasks and activities to improve motor skills, strength, balance, and coordination. They can also help patients learn how to manage daily tasks (ADLs) while living with a proprioception dysfunction. There is converging evidence that proprioceptive training can provide significant improvements in somatosensory and sensorimotor function. Retraining a somatosensory function includes any intervention aimed at improving somatosensory modalities. These intervention methods are as follows:
• Education
• Repetitive practice and feedback in detecting, positioning, discerning or recognizing different sensory stimuli, pressure or objects
• Proprioceptive training
• Balance training (Unpredictable conditions in external stimuli such as unstable floors)
• Dual task training (eg when there is no visual feedback)
• Somatosensory stimulation,





